So we’ve covered bony pain and compartment syndrome next up is tendinopathy.
The most likely to cause shin pain is Tibialis Posterior Tendinopathy, often termed Posterior Tibial Tendon Dysfunction so we’ll call it PTTD for short. There is also Peroneal Tendinopathy, it’s much less common so I might cover it in a later blog if people request it.
PTTD
This diagram shows 2 things. Firstly the rough route of the Tibialis Posterior tendon as it winds round under the medial malleolus (bone on the inside of the ankle). Secondly, that I really can’t draw!
Tib Post has a couple of key roles, it helps to maintain the arch of the foot and also acts in ankle inversion (turning the ankle in) and plantarflexion (pointing the ankle down).
Similar to Achilles Tendinopathy which is detailed here, PTTD can be caused by overload to the tendon during running or other activities. Gradually the tendon structure changes and becomes less efficient at managing load and a vicious circle develops.
Early signs of PTTD include pain, usually felt along the tendon as it runs along the lower part of the tibia and around the inside of the ankle, and crepitus (a clicking or creaking sensation felt within the tendon with movement). As the condition progresses you may notice weakness with plantarflexion – difficulty doing a calf raise on that side and loss of the normal arch on the inside of the foot (this is called flat foot deformity)
PTTD has 4 stages;
- Pain and swelling along the length of the tendon but you are still able to do a single leg calf raise and there is minimal flat foot deformity
- Pain and swelling remain, you are now unable to do a single leg calf raise and there is noticeable flat foot deformity but this can be temporarily corrected passively (I.e. if your Physio/ GP manipulates the foot). At this stage Tibialis Posterior tendon isn’t functioning effectively as it is enlarged and elongated.
- The progression from stage 2 to 3 means a more severe flat foot deformity that can no longer be corrected.
- The deltoid ligament (on the inside of the ankle) fails and the ankle joint itself becomes involved, and begins to collapse inward completing an overall picture of an overpronated foot and ankle.
I’ve heard several variations of these stages and it’s worth noting not everyone will experience PTTD the way the textbook describes. Some authors also divide stage 2 into a 2a and a 2b, more details here. Chronic tendinopathy is not thought to be an inflammatory process but instead a gradual degeneration of the structure of a tendon. As a result it can, at times, be a relatively pain free process. It isn’t unheard of for someone’s first symptom of a chronic tendinopathy to occur when the tendon ruptures, which is the final stage of degeneration. In clinic I sometimes see patients with the signs of Achilles tendinopathy (thickening of the tendon with evidence of nodule formation) but with no pain. It seems quite common that patients have a degenerate Achilles which ruptures (usually with a trauma being the straw that broke the camel’s back) and this is the first they know of it.
Carol, (Jeepers from the RW Forum) had a similar experience with her Tibialis Posterior. She’s very kindly agreed to share her story with RunningPhysio, you can read that here.
Causes of PTTD
Anything that increases the load on the Tibialis Posterior tendon above the level it can cope with can potentially cause PTTD. Regular readers will spot many of the usual suspects;
Training Error – discussed at length elsewhere in this blog (and others), training error is reportedly involved in 60-80% of tendon problems in runners. Any change in training including distance, speed, hill work, interval training etc should be a gradual process to allow the body to adapt. If it isn’t you run the risk of overloading structures and causing problems. Plan your training carefully and include rest days to allow tissues to strengthen and adapt to the load placed on them by running.
Biomechanics – if you already have a flat foot or tendency to overpronate this places greater load on tib post. Having a gait analysis or seeing a podiatrist may help prevent this. You can also try “off the shelf” orthotics but if you have limited knowledge of foot posture it can be hard to make an educated choice.
Footwear – a shoe that prevents overpronation and has a reasonable heel-to-toe drop (explained nicely here by runblogger) should in theory reduce load on tib post. I say in theory as I don’t think the research has anything conclusive on this matter. It’s hard to advise on shoes as there are so many different views on this but I’d choose a stability or motion control shoe for this over a neutral or minimalist shoe.
Muscle weakness – the main power for plantarflexion usually comes from the gastrocnemius and soleus muscles in the calf. If these are weak it could place extra load on tib post. If it’s not painful try doing repeated calf raises on each leg, count how many it takes until you reach fatigue. Compare each side. The difficulty with this is that beyond stage 1 of the condition it’s likely you may not be able to calf raise on one leg.
Reduced flexibility – tight calf muscles have also been linked to extra load on tib post. As mentioned in this very detailed article on overuse injuries.
Poor movement control – poor movement control and overpronation go hand in hand. Lack of control at the hip, knee and ankle can all play a part. Assess your single leg balance and single knee dip. Look for the hip adducting (moving towards the other leg) or the ankle rolling in. If you see a control problem try and slow the movement down and do it as an exercise. You may need some support at first until your control improves. Details on improving your movement control are here.
Altered running form – linked with strength and control, running form can place extra load on certain areas. You may be able to reduce pain by reducing your stride length. Again gait analysis may be helpful. With runners I often assess impact control, it’s not easy to do with the naked eye but if you use slow-mo video you can often see issues to address. One of the hardest parts of Physio for runners is making the transition from strength, flexibility and control work to functional change. With guideance and practice you can improve impact control. The aim is that the force of impact is then more evenly distributed through the tissue rather than overloading certain areas.
A rehab approach from the research
Kulig et al. 2009 looked at orthotics, concentric exercise, stretches and eccentric exercise for PTTD. They found a combined approach of custom made orthotic (insoles to improve foot and ankle position), calf stretches and eccentric exercise was most effective. It resulted in the biggest improvement in pain and function and also resulted in the tendon being able to work against the greatest resistance (compared to the other treatment regimes).
Concentric exercise is a contraction that involves a shortening of a muscle. Eccentric exercise is a controlled lengthening of a muscle. Take a calf raise for example, as you push up on your toes the calf muscles shorten and work concentrically to lift you against gravity. Next as you lower, the calf muscle lengthens and controls the lowering process. This is eccentric muscle activity, without this controlled lowering your heels would just drop to the floor after your calf raise.
This is just one, relatively small study but it gives us an indication on how to approach rehab. They used a special machine to load tib post but I think you could replicate it with resistance band. I’ll upload a video to show you the exercise when I get a mo. In the meantime this is how I’d do it;
- In sitting with your heel resting on the floor and a resistance band around your foot as if you were resisting pulling the foot in against the band
- Hold on to the band but make sure there is minimal resistance.
- Turn the ankle in and down, move as far as comfortable.
- Now use your hand to place as much stretch as comfortable on the band
- Keep that stretch on and move your foot back to it’s usually resting position, keep the resistance on throughout.
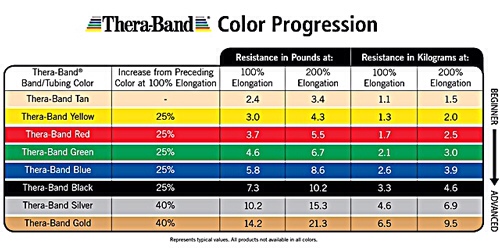
The study by Kulig et al. started with a resistance of 0.9kg and progressed up to as much as 9kg with the patients gradually increasing the load each week providing they could do 3 sets of 15 reps with ease and minimal or no pain. The exercises were repeated twice daily as 3 sets of 15 reps separated by a 1-2 minute rest. Resistance band can provide a very similar range of resistance;
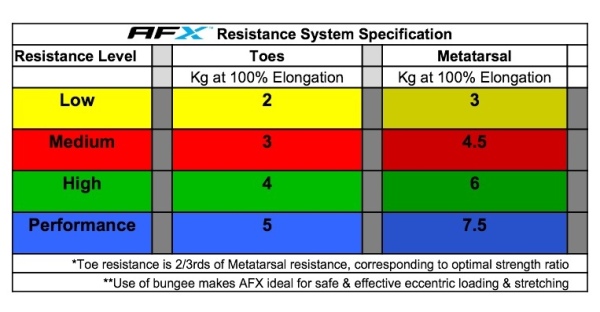
Note 100% elongation means using a 1metre band stretched to 2metres. 200% would mean stretching the same band to 3metres. More details here. Other types of resistance band are available. There is also a new product available in Canada and the US (but yet to be available in the UK) called AFX. It’s been designed to strengthen the ankle and intrinsic muscles of the foot. The resistance profile is similar to resistance band so could be used for rehab of PTTD;
For more information on this product check out their website or chat to Matt on @afxonline on Twitter. It’s an innovative alternative to resistance band and we have full details in our RunningPhysio review here. Here is how you’d use it for PTTD;
More from Kulig et al. 2009…..Calf stretching in this study consisted of gastroc and soleus stretches held for 30 seconds. 3 of each stretch, done twice daily. Details and pictures of the stretches can be found in the appendix at the end of the article. The results were achieved after doing this programme alongside the use of orthotics for 12 weeks.
So once again with tendinopathy we’re seeing a combination of determining potential causes, offloading and selective gradual reloading to strengthen and allow return to function. This is three part shin pain blog that actually started as a one part blog is now set to become a four parter! In the final section I’ll look at neural and vascular causes of shin pain.


Another great blog Tom. These will keep me sane on my 8 month ITU stint!
Cheers Stu. So when are you writing your guest blog then??
Pingback: Jeepers! What have you done? (A personal post on tib post) | RunningPhysio
Pingback: Top 3 solutions for common running injuries | RunningPhysio
Thanks for a clearly-written, researched-based post!